Introduction
In newly diagnosed multiple myeloma (NDMM) patients (pts), induction followed by high-dose chemotherapy and autologous stem cell transplantation (ASCT) remains the standard of care. The addition of an anti-CD38 antibody, daratumumab, to an established frontline protocol based on bortezomib, thalidomide and dexamethasone (D-VTd), improves efficacy but could hamper peripheral blood stem cell collection (PBCS).
Methods
The aim of our study is to evaluate the possible impact of the addition of daratumumab to induction therapy prior to ASCT on PBCS and hospitalization parameters a real-world population with NDMM.
We hereby, retrospectively analyzed 28 NDMM pts who received 6 cycles of D-VTd as induction therapy before ASCT and compared them with a consecutive series of 32 VTD-treated NDMM pts who were matched for cytogenetic abnormalities and age, managed at the Hematology Department of Sapienza University in Rome.
Results
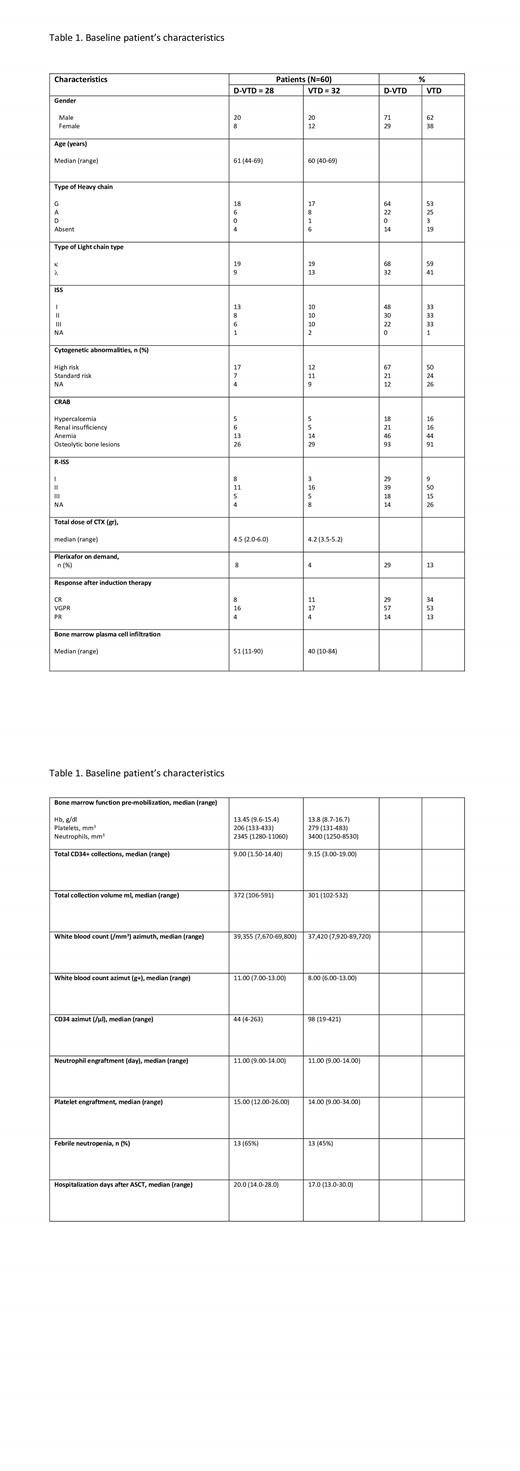
Patient baseline characteristics were equally distributed among both groups, as summarized in Table 1.
After induction therapy, a combination of cyclophosphamide (CTX) with granulocyte colony stimulating factor (G-CSF) at standard dose of 10 mg/sqm/day was used as the first mobilizing regimen attempt in both groups.
The median time between the last day of induction therapy and the first day of mobilization therapy was 30 days for D-VTd groups and 22 days for VTD groups (p=0.041).
Overall, 94% of pts treated with VTd met the desired collection goal after first mobilization therapy, compared to 68% of pts treated with D-VTd (p=0.01). In the VTd arm, 1 pts required a second mobilization attempt, and 1 pts required a further one. In the D-VTd arm, 5 pts required a second mobilization attempt, and 4 pts also required a further one. Overall, 3 pts in the D-VTd arm did not meet the collection goal. In pts with impaired mobilization, plerixafor was used in 4/32 pts in the VTd arm (13%), compared to 29% of pts treated with D-VTd (p=0.195).
In the D-VTd arm, 12/28 pts (43%) had received a higher dose of CTX as mobilization therapy (3 g/m 2) compared to the standard dose of 2.4 g/m 2 in 16/28 pts (57%). Nevertheless, no difference was observed in the rate of PBSC collection at the first attempt (p=0.7). No baseline clinical or disease characteristics were observed to have negative impact on the PBSC at first mobilization attempt, including treatment response at the end of induction therapy. Nevertheless, a significantly lower pre-mobilization level of platelet was detected in the group of D-VTd treated pts (173.000/mm 3 vs 210.000/mm 3, p=0.012) that did not meet the desired collection goal after first mobilization therapy.
The median PBSC collection was 9.1x10 6 CD34+ cells/Kg in the whole cohort, with no significant difference in the two groups. A lower pre-mobilization level of neutrophils (p=0.028) and platelets (p=0.004) was observed in the D-VTd arm compared to the VTd arm, possibly reflecting prolonged daratumumab-related hematological toxicity. No significant difference was observed in the leucocyte (WBC) azimuth value in the two arms. However, the two groups reached this value on two different days. In the VTd arm the median day was 8, and in the D-VTd arm it was 11 (p=0.034). The use of G-CSF for more days did not result in an increase in CD34+ and the median azimuth value of CD34 was significantly lower in the D-VTd group than in the VTD group (p<0.001). The median collection volume from apheresis devices was significantly higher in the D-VTd group (372 ml) compared to VTd arm (301 ml) (p=0.05), possibly related to a higher WBC azimuth in D-VTd arm, resulting in a prolonged apheresis procedure. Pts receiving D-VTd had slightly delayed hematopoietic neutrophil (11 vs 14 days, p=0.030) and platelet (15 vs 14 days, p=0.018) engraftment, but no requiring a higher number of red cell (p=0.6) and platelet (p=0.3) transfusions and a longer hospitalization (20 vs 17 days, p=0.2) after the first ASCT, compared to pts treated with VTd. No difference in the two groups regarding rate of febrile neutropenia (65% vs 45%, p=0.2) and use of antibiotics (53% vs 57%, p=0.8) were observed.
Conclusions
In conclusion, frontline induction daratumumab-based therapy is likely to affect PBSC collection after first mobilization attempt, even if not clinically relevant, and potentially mitigated with higher use of plerixafor. Furthermore, the inclusion of daratumumab in pretransplant therapy regimens did not impair ASCT.
Disclosures
Petrucci:Janssen-Cilag: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Support for attending meetings and/or travel; Celgene-BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Support for attending meetings and/or travel; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Support for attending meetings and/or travel; Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Support for attending meetings and/or travel; GSK: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Support for attending meetings and/or travel; Roche: Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Menarini: Membership on an entity's Board of Directors or advisory committees.